Reading Time – 12 Minutes, Difficulty Level 1/5
The term “autoimmune” is one most people have heard at one point or another, but what does it actually mean?
About 1 in 10 individuals suffer from some form of autoimmune disease, a greater proportion being women. Although the exact cause of their occurrence is unknown, studies point to genetic and environmental factors including viral infection or medications. The diagnosis of autoimmune disorders is also increasing, however it is not understood if this is due to improvements in diagnosis methods or actual causal links to aspects of our environments.
Autoimmunity can not only affect any individual, but can also impact just about any area in our bodies. Some unique examples of autoimmune disorders include, but are not limited to:
Celiac disease – damages lining of the small intestine
Graves disease – causes overactive thyroid and hormone dysregulation throughout the body
Rheumatoid arthritis – leads to over inflammation of the joints
Type 1 diabetes – damage to insulin producing cells within the pancreas
Multiple sclerosis – damage to proteins important for nervous system functions
What is an autoimmune disorder?
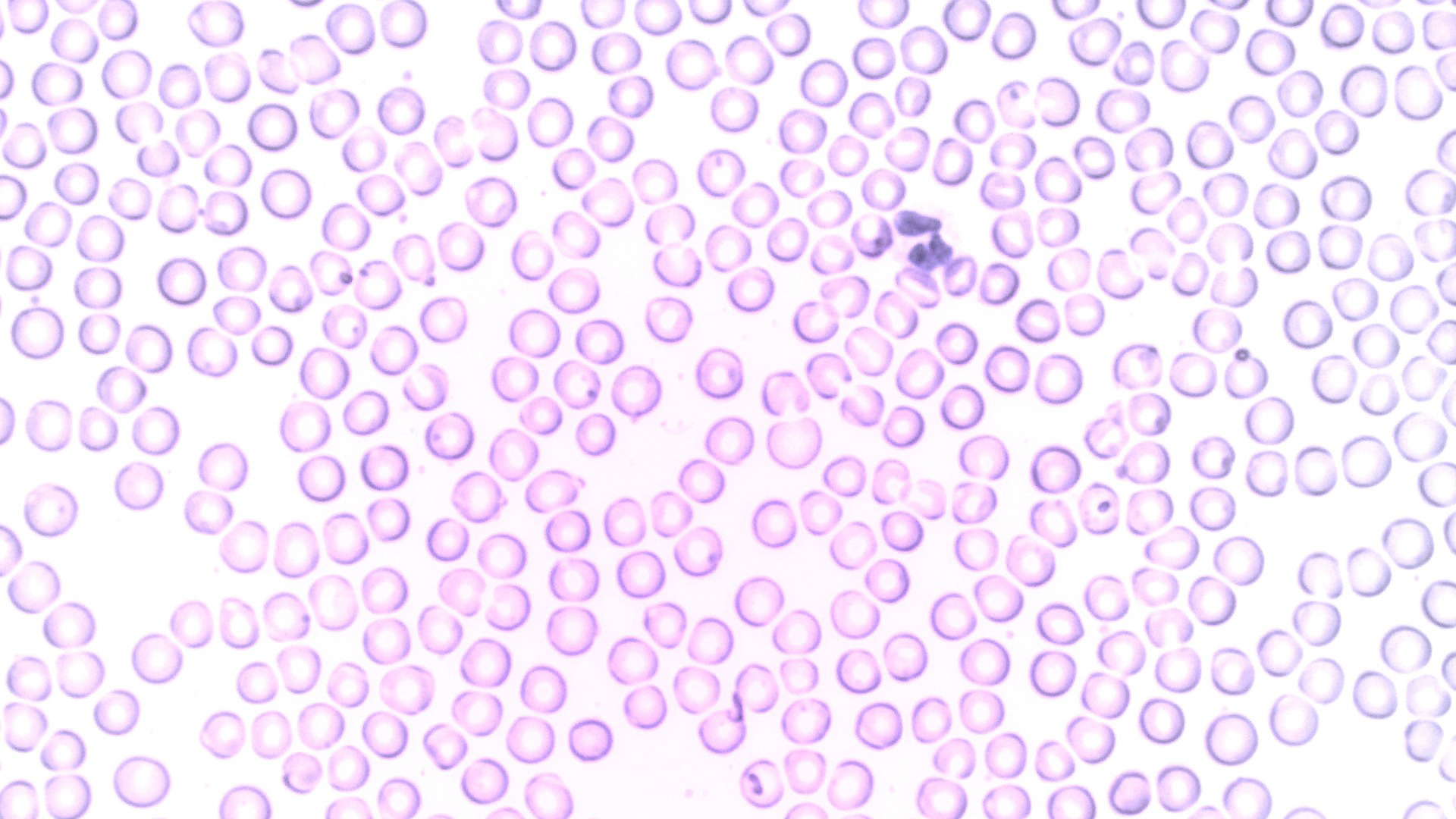
The basic metric for autoimmune classification is when our immune system begins to attack our own cells. In healthy individuals, immune cells can discern the differences between our cells and invading pathogens or disease. In the case of autoimmunity, immune cells see our healthy cells as a danger, and begin to attack them.
Think of it as if the military began attacking its own country rather than protecting against potential invaders. As you can imagine, similar to if our own militaries began destroying our cities, when our immune cells attack our healthy tissues lots of local and widespread damage can occur. The damages can confer a huge plummet in quality of life for an individual and may even threaten their life if left undiagnosed or untreated.
Additionally, autoimmune diseases are typically unregulated and do not experience the same immune suppression we see in healthy immune reactions. This means that not only are our tissues being attacked by their assigned protectors,but the attacking cells aren’t ever told to “back off”, and can continue their attack for as long as they’d like.
What causes these diseases?
Although specific causes for each autoimmune disease have not been discovered yet, it is of general consensus that there are both genetic and environmental components playing a role in the development of autoimmunity. Via studies of genomic data as well as the prevalence of certain autoimmune diseases within families, it is clear that several genes can be attributed to aberrant immune function.
Similar to any multi-gene disorder, however, it is not genes alone that lead to disease occurrence. Environmental factors including viral infection or medications may cause the development of autoimmune reactions, but more research in this field is required. The diagnosis of autoimmune disorders is also increasing, however it is not understood if this is due to improvements in diagnosis methods or actual causal links to aspects of our environments.
Graves disease
A perfect example of how autoimmune disorders can cause serious downstream effects is Grave’s Disease. In this case, immune cells attack the thyroid gland, leading to the overproduction of thyroid hormones. The thyroid gland sits in the front of your neck just under the larynx (Adam’s apple). This oddly beautiful gland resembles a butterfly, with the two wings extending past each side of your trachea, or windpipe.
Thyroid hormones, triiodothyronine and thyroxine, are responsible for the regulation of energy consumption, heart rate, body temperature, speed of digestion, brain development (in infants, of course), muscle contraction, and more. The regulation of thyroid hormone production is therefore extremely important for regulating many processes in our bodies.
An individual with Grave’s Disease will suffer damage to the thyroid, leading to a dramatic increase in thyroid hormone production, known in clinical terms as hyperthyroidism. This overproduction can lead to symptoms such as unintentional weight loss, rapid or irregular heart rate, heart palpitations, sweating and heat sensitivity, low energy, muscle weakness, trouble sleeping, anxiety and irritability, heart palpitations, and more.
Additionally, an individual with hyperthyroidism may present with an enlargement of the thyroid gland which can be visible as swelling in the neck. In addition to hyperthyroidism, Grave’s Disease may also cause eye issues (blurry vision, irritated eyes, or light sensitivity) or skin problems.
Grave’s Disease is the most common cause of hyperthyroidism and affects about 2-3% of the global population, mostly women over the age of 30. Risk factors for the autoimmune disease include a family history, indicating genetic components, as well as the presence of other autoimmune disorders.
The mechanistic cause for Grave’s Disease and the overstimulation of the thyroid gland is the production of an antibody called thyroid-stimulating immunoglobulin (TSI). This antibody is not produced by the immune cells of healthy individuals, but individuals with an autoimmune reaction to thyroid tissue will produce it through means beyond the scope of this article.
SI will bind to the surface of the thyroid cells and activate their intracellular processes, driving the production of thyroid hormones. Essentially, TSI mimics the normal stimulatory signals our body is meant to produce, but there are no negative feedback loops to turn off the signal. Genes involved in immune responses as well as genes involved in thyroid cell surface proteins (which is what TSI will bind to), have been implicated in the occurrence of Grave’s Disease. Like most autoimmune disorders, however, the exact cause of Grave’s Disease has not yet been elucidated.
Treatment of this disorder varies depending on severity, duration or persistence of disease, and age of the patient. The treatment preferred for young patients, pregnant women, or patients with milder hyperthyroidism is the administration of drugs which reduce the release of thyroid hormone. If the patient’s symptoms worsen, do not improve, or persist past the treatment regimens, a physician may opt for treatments which destroy the thyroid gland. Destruction of the gland can be achieved through radioactive iodine therapy or surgical resection. These treatments carry a large burden on the patient because they will be required to supplement their body with thyroid hormone indefinitely.
Type 1 diabetes
Diabetes is an extremely common disease with hundreds of millions of individuals impacted worldwide. Type 1 diabetes, however, only exists in about 5% of diagnosed individuals, and is typically diagnosed in children or adolescents. In patients with type 1 diabetes, their immune system attacks and damages the pancreas. This autoimmune reaction severely diminishes the ability of specialised pancreatic cells to produce insulin. This insulin deficiency results in the accumulation of glucose, or sugar, in the blood because it is unable to enter the cells and be used for energy. The standard treatment for individuals with diabetes, then, is the daily administration of insulin to ensure glucose enters the cells and cellular mechanisms can continue without issue.
Untreated type 1 diabetes and thus an increase in blood glucose levels can result in blurry vision, low energy, unintentional weight loss, and increased hunger and thirst. Chronically low insulin levels may lead to diabetic ketoacidosis, which is a life threatening condition in which the body, in a desperate attempt to produce energy, breaks down fat stores at high rates.
The breakdown of fat results in the release of ketones, which is an alternative cellular fuel to glucose. Ketones, in healthy situations, are an essential source of fuel for our bodies in the absence of glucose; however, in the case of a diabetic person, the high levels of ketones in the blood impart toxicity by making the blood too acidic.
We often hear about diabetes in the context of type 2 diabetes which, despite similar symptoms, is actually very mechanistically different from type 1. Firstly, type 1 diabetes is an autoimmune disorder in which the immune system is attacking the pancreatic cells, perturbing their ability to secrete insulin. Type 2 diabetes is, generally speaking, caused by a cellular resistance to insulin, meaning to get the required amount of glucose into the cell, your body needs to produce more insulin.
So, the pancreas of a type 2 diabetic is still able to produce insulin, but not able to produce the amount required to import the glucose into the cells. Type 2 diabetes is in itself a very complex and prevalent disease, but is not classified as an autoimmune disorder because there is no immune dysfunction observed to be causing the disease.
In the case of type 1 diabetes clinicians and scientists are still working to elucidate the full causes for its onset. It is clear, however, that there are both genetic and environmental components associated with the risk of disease, similar to many autoimmune disorders in our populations.
Type 1 diabetes treatment is based on the necessity for insulin administration when blood glucose concentrations get too high. Many individuals with diabetes carry glucose monitors which prick their finger to measure the concentration of sugar in their blood, and based on the concentration, self administer insulin via an insulin pen, needle and syringe, or insulin pump.
Recently, patients with type 1 diabetes are now able to opt in, based on their physician’s recommendation and analysis, for an “artificial pancreas”. This technology allows a patient to erase the burden of manual glucose monitoring and insulin administration. The artificial pancreas is composed of a continuous glucose monitor which controls the administration of insulin via an insulin pump. The glucose monitor is coded with a specialised algorithm that can calculate glucose concentrations, and then determine if a dose of insulin is needed, automatically causing the insulin pump to administer the medicine into the patient, without them having to do much work.
Multiple Sclerosis
When immune cells begin attacking a protein called myelin, the individual can develop multiple sclerosis (MS). Myelin is the protein that sheaths our neurons (cells of our nervous system) and spinal cord. Damage to these protective proteins leads to slower nerve signals, causing impaired brain and spinal cord function. This impairment ultimately leads to fatigue, issues with balance and coordination, muscle weakness and spasms, and more.
Individuals with this disease may also experience memory issues, difficulty walking, and an inability to control bowel or bladder functions. Currently, there is no cure for this disease and treatment only serves to slow the progression. Common treatments for MS include medications targeted at reducing flare ups and physical therapy to help maintain strength.
In the event of a flare up of symptoms, a physician may prescribe high doses of corticosteroids, which reduce inflammation and slow the damage to myelin. There is some evidence that healthy diets, exercise, and stress management can help improve the symptoms of MS and help slow the progression of disease.
Like the other autoimmune diseases discussed in this article, scientists still don’t know the exact cause of MS. Of course, there are some genetic elements that play a role in the development of MS, but the specific associated genes have not yet been discovered. The current literature suggests that many environmental factors such as exposure to specific viruses (Epstein-Barr, for instance) and where you live in relation to the equator may play a role.
The distance a person lives from the equator may play a role in the context of sun exposure because disruptions to circadian rhythms (biological “clocks” that correspond to natural light patterns) or vitamin D deficiency increases the risk of developing MS. It is also interesting to note that individuals who have disruptions to their circadian rhythms on a regular basis, such as shift workers, have a higher associated risk of developing MS. This is, of course, not to say that shift work will cause MS development, but is a measure of the increased risk these individuals have in comparison to people who work a 9-5, for instance.
Concluding remarks
Autoimmune diseases are extremely variable and can impact anyone of any age or sex. The treatments are also highly variable, but typically rely on treating symptoms of disease rather than the cause. Treating the cause, in some cases, may actually translate to deactivating or weakening our immune systems, which is a highly unfavourable method of action. To go back to our previous analogy, if the military begins attacking its own cities, and the government wipes out or weakens the military, the country is now extremely vulnerable to outside attacks. In the case of autoimmunity, it is often better to rebuild the city or barricade the buildings (treat the symptoms), than to abolish the protective force of the country (weaken the immune system).
With the advancements of immunological research and as our understanding of autoimmune disorders increase, hopefully we will begin to develop preventative protocols for those at risk of developing certain autoimmune disorders. The cellular events which lead to immune system dysfunction are fascinating, and I am extremely excited to learn what new advancements in this field will arise within the next few years.
References
Autoimmune disorders. Mount Sinai Health System. (n.d.).
Cleveland Clinic medical. (n.d.). Multiple sclerosis (MS): Symptoms, causes, diagnosis & treatments. Cleveland Clinic.
Graves disease – symptoms, causes, treatment: Nord. National Organization for Rare Disorders. (2023a, June 23).
Graves disease – symptoms, causes, treatment: Nord. National Organization for Rare Disorders. (2023b, June 23).
Mayo Foundation for Medical Education and Research. (2022, November 30). Hyperthyroidism (overactive thyroid). Mayo Clinic.
Tenth edition. IDF Diabetes Atlas. (n.d.).
U.S. Department of Health and Human Services. (n.d.-a). Graves’ disease – niddk. National Institute of Diabetes and Digestive and Kidney Diseases.
U.S. Department of Health and Human Services. (n.d.-b). Type 1 diabetes – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases.

I’m a first year Masters student at Queen’s University, Ontario, Canada studying Immunology and Cancer, following on from completing a BSc at the University of Guelph, Ontario.
I have a passion for Molecular Biology, with a particular interest in the use of modern molecular techniques to treat and cure disease.